“Unprecedented, irreversible, crisis.” These are the words that headlines are relying on to communicate the risk that climate change is posing to humanity. Even so, it can be difficult to fathom how it will affect our everyday lives and society as a whole. How will climate change affect health care and why should nurses specifically care?
- Increased burden of disease
Most obviously, climate change will increase respiratory illness, cancers, heat related illnesses, acute injuries, and communicable diseases, as well as compress available services for treatment.
Hotter weather and increased air pollution is predicted to cause greater rates of respiratory illnesses and cancers, as well as acute illness during extreme weather events. During the “heat dome” in Canada in June and July of 2021, 445 people died of heat related illness (HRW, para. 6) in a 2 week period. This type of weather event is becoming more common and is expected to routinely stress our healthcare system (Ebi et al, para 47). A longer wildfire season is expected to worsen air quality as well as cause more acute injuries. Outdoor air pollution is a known carcinogen. Public health agencies focus their campaigns on personal responsibility, yet air pollution is the second largest cause of lung cancer after smoking, at 14.1% of cases (Turner et al, para 23). This number could rise significantly as air quality worsens globally.
Rising temperatures are causing larger territories for pathogens that used to be contained by weather, climate, and infrastructure, like malaria. Malaria is already a leading cause of death, especially for children and babies. As we become less capable of handling the rapidly changing climate and weather, diseases like malaria are expected to come back in places that thye are believed to be eradicated, like the United States. There is also the issue of displaced persons. As we have seen in the recent refugee crisis out of Ukraine, different parts of the world have unique health challenges. Ukraine has one of the highest rates of drug resistant Tuberculosis in the world, and now millions of their citizens have been forced across borders (Holt, para 4). As we see more refugees and displaced people, we can expect that globally healthcare workers will be exposed to diseases that they may be susceptible to, and also may not be experienced in treating.
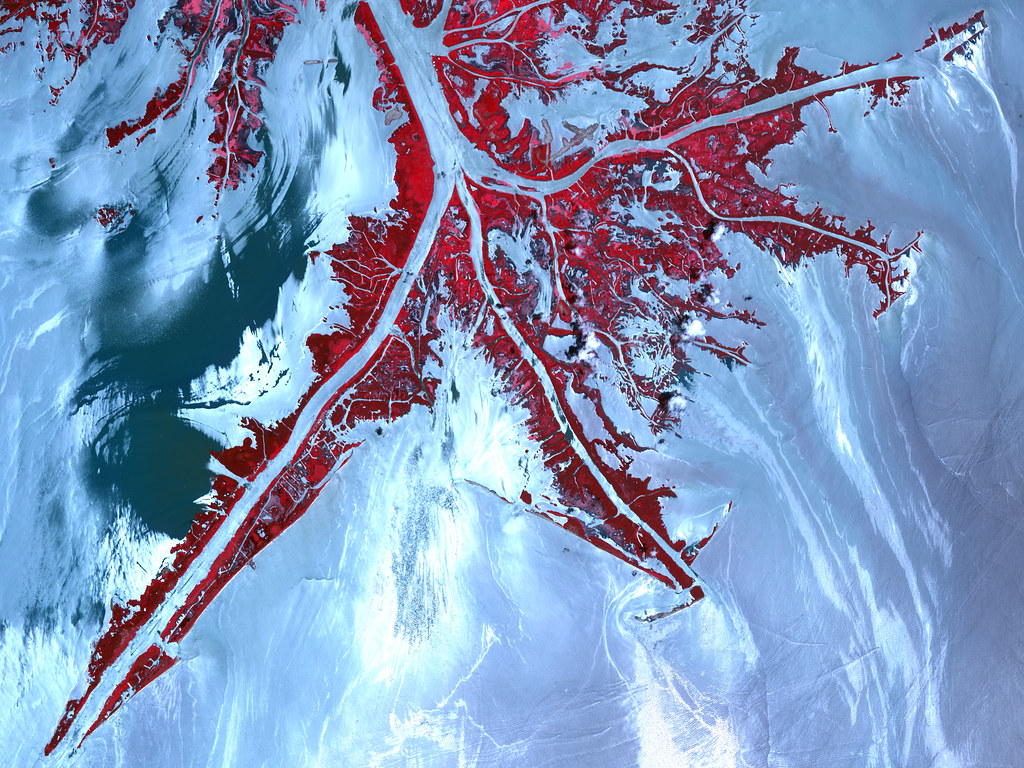
Permafrost holds pathogens like anthrax, influenza,and the bubonic plague that humans will be exposed to as melting ice delivers them into the environment. Siberia experienced an anthrax outbreak that was linked to melting glaciers in 2016, from a long frozen reindeer carcass (Doucleff, para 2). This led to at least one death, evacuations, culling of reindeer, and a large public health response. Increased temperatures also mean that vectors could expand their territories, and the territories of the diseases they carry.
Longer stretches of warm temperatures have already increased allergy season by up to 27 days, and poor air quality increases risks of severe asthma attacks (AAFA, para 2). These are diseases that can cause permanent lung damage and lead to greater need for healthcare services in old age.
Increased burden of disease means a greater strain on the healthcare system, and a greater strain on nurses. It can also mean ethical dilemmas and moral distress for nurses when the system is unable to adequately care for the volume of patients.
2. Civil unrest
Civil unrest is expected to increase as areas struggle to cope with famine and drought, as well as the pervasive effects of extreme weather such as economic difficulty, jeopardized housing and infrastructure, and increased burdens on still operational systems as they take on more displaced persons. We usually focus on the immediate health effects of pollution and heat waves, but these social issues are a serious threat to healthcare systems worldwide. This type of social upheaval and civil unrest affects every single social determinant of health, which already have the power to lower life expectancies by 18 years irrespective of climate change (WHO, para 6).
Nurses will see these challenges in healthcare as societies struggle to care for their most vulnerable citizens and the healthcare system as a whole manages an increased patient load with fewer resources.
3. Triaging society
We have made great strides recognizing how mental health and wellbeing impacts people’s lives. However, we must recognize that when push comes to shove, it will always be relegated below physiological and safety needs like housing, food, and clean water. Climate change and the associated stress it will place on society threatens to undo decades of progress in the mental health as we are forced to confront more direct threats to lives.
Climate change threatens the provision of universal healthcare, through lack of access and increased burden of disease (WHO, para 1). Additionally, it threatens to stress healthcare workers out of their professions. We saw this during our most recent global health crisis, as healthcare professionals quit in huge numbers, further stressing the ones that remained. We are also threatened with a lack of progress. During times of emergency, less time, resources, and brainpower can be put into issues that currently are heavily researched, like Alzheimers, autoimmune disease, and gene therapy. Climate emergencies and extreme weather events threaten lab equipment and supply chains, as well as energy usage for noncritical activities. Well these are all diseases that threaten and change lives, like mental health, they will be deprioritized as we face immediate existential threats.
For nurses, this means less time and energy to spend on patients who are not deemed critical, and more difficult decisions to make on how to spend time and resources.
Nursing is a role that meets people where their private lives intersect with public policy. This means that nurses need to be aware of how the world outside their workplace is impacting the lives of their patients and trends in healthcare. Climate change is like nursing in that it will bring people’s personal lives into conflict with global activities. As a profession, we need to be prepared to tackle the challenges that a changing climate is bringing us, through direct increases in illness and injury and the indirect consequences of destabilized societies and barriers in care. Additionally, we need to recognize that we ourselves will be impacted by the changing climate with our communities, and may ourselves be dealing with poor health, civil unrest, and lack of access to services. Nurses everywhere should recognize that their role will be challenged by the upheaval of climate change, and prepare to respond to this while upholding the values of their profession.
Asthma and Allergy Foundation of America. (2021). Extreme Allergies and Climate Change. Retrieved March 27th, 2022 from https://www.aafa.org/extreme-allergies-and-climate-change/#:~:text=Rising%20temperatures%20caused%20by%20climate,11%20to%2027%20days%20longer.
Ebi, K. L., Berry, P., Hayes, K., Boyer, C., Sellers, S., Enright, P. M., & Hess, J. J. (2018). Stress Testing the Capacity of Health Systems to Manage Climate Change-Related Shocks and Stresses. International journal of environmental research and public health, 15(11), 2370. https://doi.org/10.3390/ijerph15112370
Holt, E. (2022). Tuberculosis services disrupted by war in Ukraine. Retrieved March 27th, 2022 from https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00214-6/fulltext#articleInformation
Human Rights Watch. (2021). Canada: Disastrous Impact of Extreme Heat. Retrieved March 27th, 2022 from https://www.hrw.org/news/2021/10/05/canada-disastrous-impact-extreme-heat#
Turner, M. et al. (2020). Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. Retrieved March 27th, 2022 from https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21632
WHO. (2021). Social Determinants of Health: Health Equity. Retrieved March 27th, 2022 from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
WHO. (2021). Climate change and health. Retrieved March 27th, 2022 from https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
Yarzábal, L.A., Salazar, L.M.B. & Batista-García, R.A. Climate change, melting cryosphere and frozen pathogens: Should we worry…?. Environmental Sustainability 4, 489–501 (2021). https://doi.org/10.1007/s42398-021-00184-8